Several international organisations recommend Mohs surgery, including the prestigious National Comprehensive Cancer Network (NCCN). Mohs gives you the best chance of treating your skin cancer correctly the first time.
It is most commonly used for the removal of squamous cell carcinomas (SCC) and basal cell carcinomas (BCC), however, numerous other types of cancers can be removed by this technique.
What are the key benefits of Mohs surgery for Skin Cancer?
Most precise
The histological analysis undertaken with Mohs is a lot more accurate than routine pathology analysis. Mohs examines 100% of the tumour margin, compared to often less than 5% with a routine examination.
Highest cure rate
Because Mohs surgery for skin cancer is a lot more precise, it is less likely to leave residual skin cancer cells in the body meaning a higher cure rate – of up to 99%.
Best outcome
As it is more precise, we can keep the surgical site/defect smaller, maximising the preservation of healthy tissue. This optimises the cosmetic result and makes for an easier healing process.
Patient-centred
We can confirm histologically that the skin cancer has been removed on the same day as the surgery. This avoids having to repeatedly return to the clinic to undertake further surgery to remove residual cancerous tissue.
The Process: Mohs Surgery for Skin Cancer
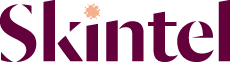
01.
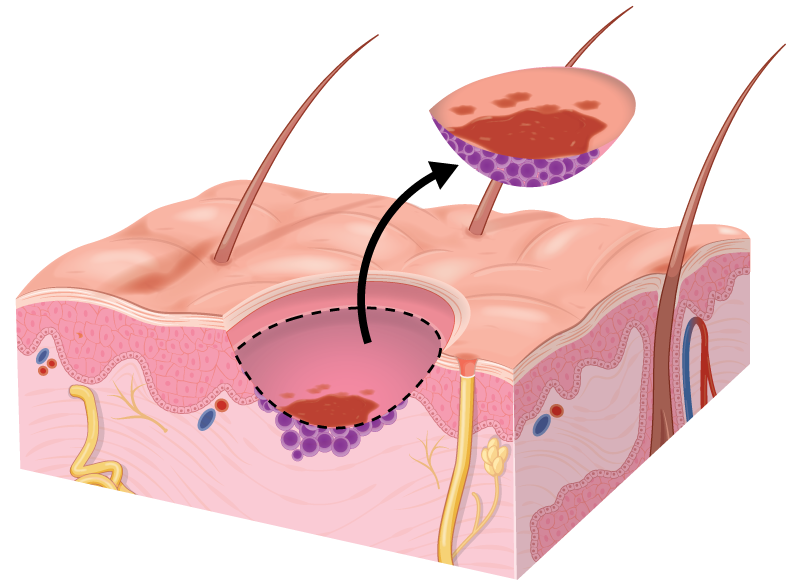
The roots of a skin cancer may extend beyond the visible portion of the tumour. If these roots are not removed, the cancer will recur.
02.
Local anaesthetic is injected to numb the area completely. The first layer of tissue is surgically removed with a narrow margin around the visible tumour. The wound is bandaged temporarily while lab work begins.
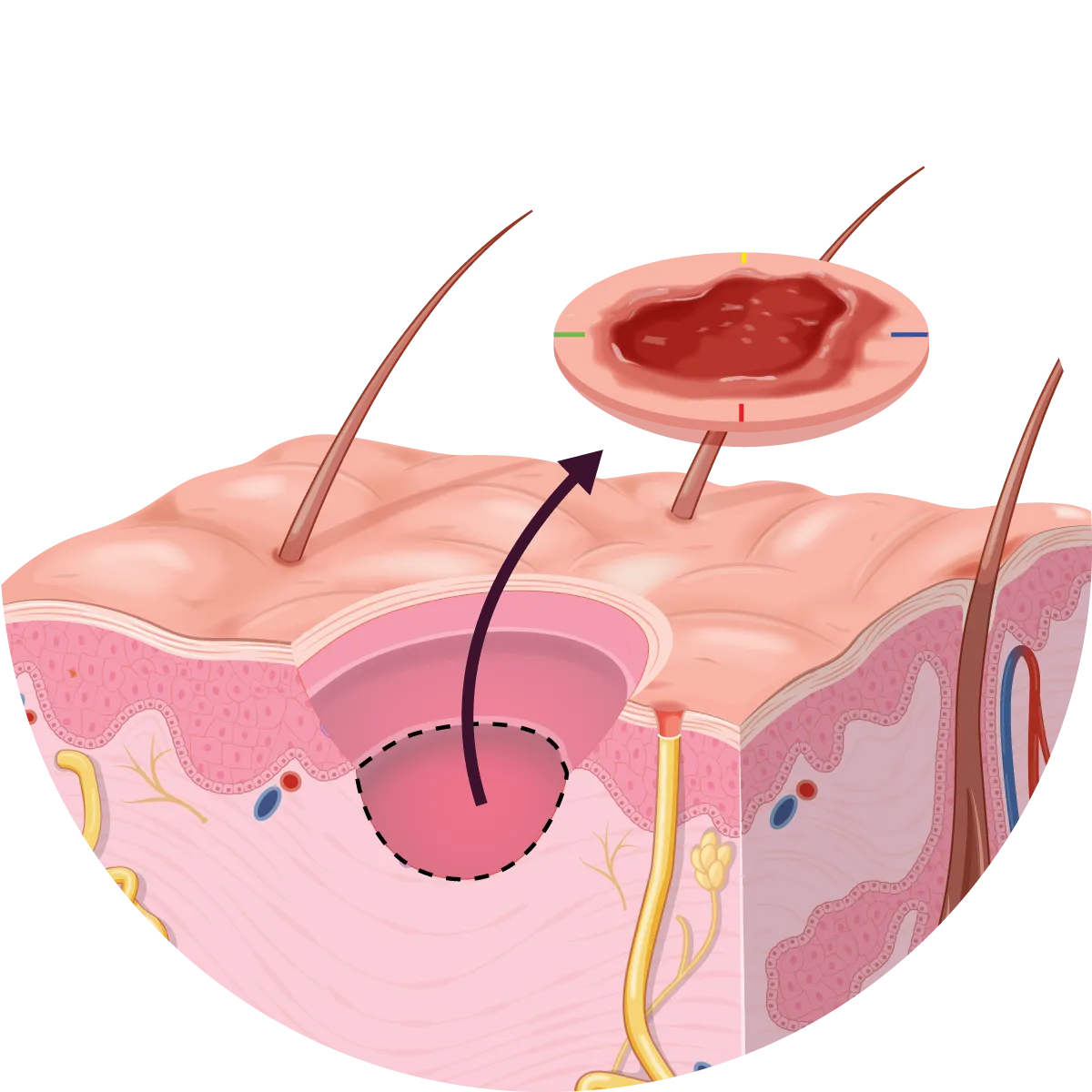
03.
The surgeon creates notches in the specimen, colour-codes them with dyes, and draws a map of the surgical site.
04.
In the lab, the tissue is frozen and very thin horizontal slices are cut, placed on microscope slides and stained for examination.
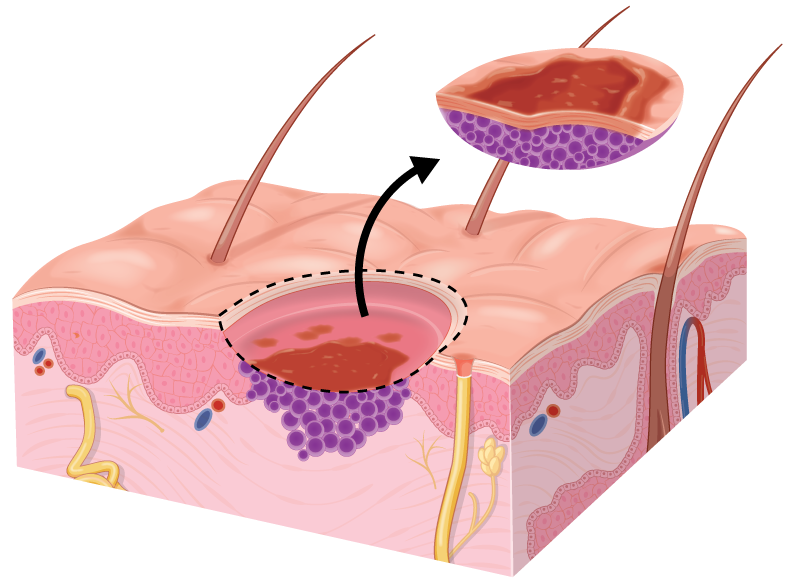
05.
Using a microscope, the surgeon examines the undersurface and edges of each tissue section for any evidence of remaining cancer.
06.
If cancer cells are found under the microscope, the surgeon marks their location on the ‘map’ and returns to the patient to remove another layer of skin – but only from the precise location where the cancer cells remain. This process is repeated until there is no evidence of cancer remaining.
07.
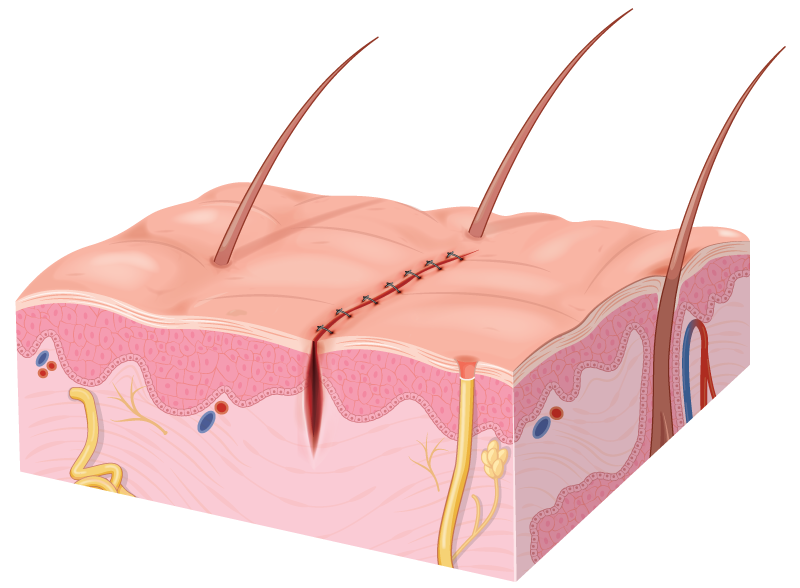
The wound may be left open to heal or closed with stitches, depending on its size and location. In most cases, the surgeon will repair the wound immediately after obtaining clear margins. In some cases, the wound may need reconstruction with a flap or skin graft.
Is Mohs surgery a new technique? Why haven’t I heard about it?
The background theory and concepts were developed by Dr. Frederic Mohs during the 1930s. It wasn’t until further refinement of the technique that it started to become more widely accepted in the 1970s and 1980s.
Mohs surgery has been available in New Zealand since the 1990s. It is offered at some public hospitals, however, it is heavily rationed.
Despite its common use and its superior outcomes, many people are unaware of the technique.
Is Mohs surgery cost-effective?
Mohs surgery does tend to have higher up-front costs due to the extra precision and analysis required. However, because of the higher accuracy, there are fewer recurrences of skin cancers after Mohs surgery, meaning fewer repeated surgeries are required to eradicate the cancer.
This not only reduces the long-term cost of treating skin cancer, but it also means better outcomes for the individual affected as they don’t have to suffer through repeated procedures.
As far as we are aware, all medical insurance companies in New Zealand see the long-term value of Mohs surgery and will usually fund the procedure (subject to individual policies). Some district health boards have also started offering Mohs surgery as an option at public hospitals, although waiting times are very long.
Why should I get Mohs at Skintel?
At Skintel we are constantly undertaking audits and reviews of our practice in our endeavour for continuous improvement.
We also take part in research to improve the process of Mohs surgery.
We are currently involved in research developing an artificial intelligence (AI) system to check the accuracy of our Mohs surgery slides. In some of our studies, this has accuracy exceeding 99%.
While there will always be a human Mohs surgeon reviewing the slides and making the final decision, this AI constantly works in the background reviewing our work.
Frequently Asked Questions
Mohs surgery is a safe surgery that can be done without a general anaesthetic. The wound site is numbed with a local anaesthetic, and most patients can drive themselves home after the procedure. With every surgery, there are some risks such as bleeding from the wound site or tenderness.
It is called “Mohs” after Frederic E. Mohs, MD (1910-2002), the pioneer and originator of Mohs Surgery. From 1929 through 1934, Dr. Mohs worked as a medical student for his mentor and zoology professor, Michael Guyer, on cancer research initiatives when he made the discovery.
Mohs surgery is the gold standard when it comes to the removal of skin cancers as it has the lowest recurrence rate of any skin cancer removal method, the highest cure rate, and the best cosmetic results.
It can take anywhere between 4 to 6 weeks for a Mohs wound site to fully heal depending on the size of the wound and if any issues occur in the healing process. Expect minimal pain upon the healing time.
Most patients will have stitches. Very seldom do we leave a wound to heal on its own, however, in some cases, this is applicable if the wound is located where it could heal well, or where you mightn’t be so concerned about scaring. Generally, Mohs patients will have a wound-check appointment with our nurses two days after the procedure, and then have their stitches removed 7 to 10 days after the procedure.
There are not really any restrictions for the day of Mohs surgery. Mohs is normally performed with local anaesthetic, meaning you can eat breakfast. We provide food and refreshments throught the day. Please all your regular medications on the day of surgery. Do not stop your blood thinner medications including warfarin, aspirin, clopidogrel and dabigatran (Pradaxa).
Mohs surgery is a procedure used to remove skin cancer. This surgery involves cutting away layers of skin and analysing each layer for signs of cancer. The process continues until there is no cancer left.
Delays to surgery can allow the cancer time to grow into surrounding healthy tissue, making removal more invasive and increasing recurrence risk. While timing varies case by case, undergoing Mohs surgery within 6-8 weeks is normally fine.
Mohs surgery is suitable for those with skin cancer located on and around the head, neck, genitals, hands and lower legs. This allows for the preservation as much of the healthy surrounding tissue as possible.
Possible adverse outcome of Mohs surgery may include: pain, discomfort, infection, bleeding and bruising.
Mohs surgery is normally performed with local anaesthetic which means you will normally be able to drive yourself home. However, if the skin cancer is close to your eyes and the dressing obstructs your vision you may need someone else to drive you home.
There are alternative treatments to Mohs surgery. However, Mohs surgery has the highest cure rate, the lowest risk of recurrence and often the best cosmetic result.
Mohs surgery is a simple and straightforward procedure. While many people get worried about medical procedures, Mohs surgery is considered a low-risk procedure.
Mohs surgery is primarily used on high risk areas such as the head and neck, hands and feet. However, because Mohs surgery keeps surgical sites smaller, it normally means lower risks of complications.
You won’t usually need chemotherapy after Mohs surgery. Mohs surgery is normally sufficient for treating most skin cancers.
Duration can vary, depending on the complexity of the skin cancer. However, the average Mohs surgery will take about 3 to 5 hours.
We normally recommend avoiding heavy lifting and strenuous activiting for at least 48-72 hours. These activities can raise your blood pressure which may encourage bleeding at your surgical site. After this time you should avoid any tension on the found for 2-3 weeks. Avoid immersing in water until the stitches are removed.
While the local anaesthetic injection may sting, most patients experience very little pain during and after Mohs surgery.
Mohs surgery has the highest cure rate (over 99%) and fewest complications for most skin cancers. Furthermore, due to the precise nature it creates a much smaller wound which usually means a better cosmetic outcome.
Most people will have stitches to close the wound after Mohs surgery – this may mean a simple side-to-side closer, a flap or skin graft. However, in some cases the wound is allowed to heal by itself (granulation).
Since its development, Mohs surgery has been refined into the most precise and advanced treatment for skin cancer, yielding success rates of around 99%.
Your Mohs surgeon undergoes a rigorous training program to become a Mohs surgeon. This includes advanced techniques for the repair of surgical wounds, including flaps, grafts and reconstruction with a focus on cosmetic outcome. As a result it is normally unnecessary to require other surgery. Furthermore, as dermatologists, Mohs surgeons are often trained in laser resurfacing which can be used after surgery to enhance the cosmetic appearance even further.
A recurrence of skin cancer following surgery can be either local or distant. Mohs surgery is the most precise surgical technique, which means it has the lowest risk compared to other treatment options.