There are a lot of factors to consider when using sunscreen:
- We recommend using it every day – even in winter and when the UV index is less than 3.
- This puts us in conflict with the World Health Organisation (WHO) and the Cancer Society, but we are not crazy dermatologists. We can justify this position with real-world evidence.
- Sunscreen does impact vitamin D synthesis, however, it’s unlikely to impact vitamin D levels.
- While there has been a move by some stating that high-SPF sunscreens are a waste of time, the evidence on this is changing and high-SPF sunscreens may be beneficial. They may help compensate for the fact that people only apply about 25% of the recommended amount.
- There have been recent studies demonstrating surprising amounts of systemic absorption of its ingredients into the blood, which we will also discuss. It is important to note that there is no evidence of harm from systemic absorption.
- There are also a lot of environmental impact reports being published, with a particular focus on marine life.
- Importantly, sunscreen only makes up a part of a sun protection regime.
- While the amount of sunscreen applied is important, intense education still does not increase quantities to the recommended amounts. A double application of the cream within 30 minutes is probably the more important strategy to encourage higher quantities of sunscreen use.
You are not using enough sunscreen unless you double apply within 30 minutes.
The physics
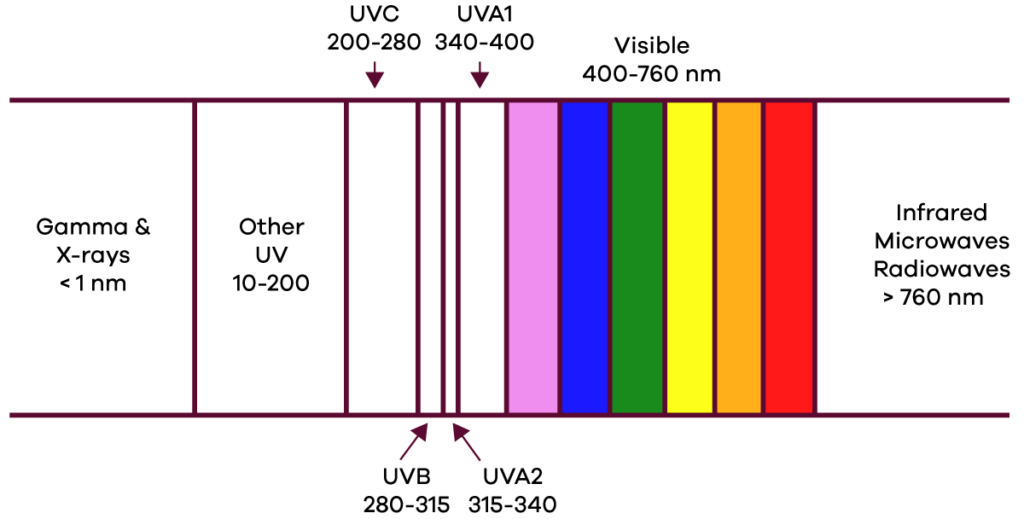
Ultraviolet radiation (290-400 nm) is the causative agent for several impacts on skin health including skin cancer and photoaging. The most significant components of UV are:
- UVB (290-320 nm) makes up about 5% of UV but is the main cause of the detrimental effects.
- UVA (320-400 nm) is responsible for 95% of UV, it can be broken down into:
- UVA2 (320-340 nm) makes up 25% of UV and can also cause the detrimental effects that UVB does.
- UVA1 (340-400 nm) is less harmful.
- UVC (200-290 nm) is also a component of UV, however, it gets filtered out by the atmosphere.
Sunscreen is made up of filters that either absorb or reflect ultraviolet radiation. Most creams contain a combination of different filters that are active against different wavelengths of ultraviolet. Filters are classified as:
- Inorganic filters: reflect or absorb UV radiation. Mainly made of titanium dioxide and zinc oxide.
- Organic filters: absorb UV radiation and convert it into heat. Made of numerous different ingredients.
Inorganic filters
Inorganic filters are mainly made of titanium dioxide and zinc oxide. They are more stable and less likely to cause skin reactions. They were initially produced with large particle sizes creating an occlusive film on the skin that was cosmetically unacceptable. Over time, this resulted in the development of much smaller nanoparticles of these same filters which are more cosmetically appealing. Inorganic filters don’t significantly absorb into the skin.
Organic filters
Organic filters are less stable and can potentially absorb into the skin. They are also more likely to cause skin irritation and allergies, although the risk is still very low. Different specific components have varying rates at which they cause reactions.
We discuss sunscreen ingredients in more detail near the bottom of this page.
The SPF of sunscreen
The sun protection factor (SPF) is a ratio that compares the minimal erythema (sunburn) dose from solar radiation of sunscreen-protected skin compared to unprotected skin. More simply, it is described by this formula:

Where MED refers to the minimal erythema dose, basically the smallest amount of ultraviolet to cause your skin to turn red (sunburn).
This means that wearing an SPF50 sunscreen takes fifty times longer to cause sunburn compared to not wearing any at all. A suncream with double the SPF rating has double the protection time (in theory). However, this is a bit misleading which we discuss in the next section.
SPF is primarily a measure of UVB protection and to a lesser extent UVA2. Broad spectrum sunscreens additionally provide protection against UVA (as well as UVB).
To validate a sunscreen, the testing involves applying it quite thick – 2 mg per square centimetre of skin (2 mg/cm2). This amount was chosen for testing as it generates the best reproducible and least variable test results. However, people don’t apply this much cream. This is where realistic applications haven’t been considered in research and thus the results aren’t a realistic view of how suncream is used.
The SPF of sunscreen in realistic applications
Several studies have shown that people generally only apply about 20-50% of the recommended amount (i.e., 0.4-1.0 mg/cm2). This of course highlights the difference between a lab environment and reality. Of course, we all live in the real world, so our recommendations need to be based on how people actually use sunscreen. Studies have even shown that those with photosensitivities who should be highly motivated to apply sunscreen correctly, still only apply it about 0.5 mg/cm2 thick.
Unfortunately, we have yet to determine the exact relationship between application thickness and SPF rating. However, most studies that have investigated this have found a relationship that is either linear or exponential with the more convincing studies suggesting a linear relationship.
It is likely that the relationship depends on the formulation of the product, so it is difficult to provide a blanket extrapolation.
Estimated real usage of SPF sunscreen
| Estimated real-world SPF for different application quantities | ||
| Labelled SPF | 0.5 mg/cm2 | 1 mg/cm2 |
| SPF 30 (linear model) | 8 | 15 |
| SPF 30 (exponential model) | 2 | 8 |
| SPF 50 (linear model) | 13 | 25 |
| SPF 50 (exponential model) | 3 | 13 |
| SPF 70 (linear model) | 18 | 35 |
| SPF 70 (exponential model) | 4 | 18 |
Is a very high SPF sunscreen worthwhile?
Over the last several years, there has been an argument that very high SPF sunscreens are a waste of time and money. The argument centres around the theoretical effectiveness of blocking UVB light and the minimal difference between SPF30 and higher sunscreens.
- SPF15 blocks 94% of UVB
- SPF30 blocks 97%
- SPF50 blocks 98%
- SPF100 blocks 99%

Real-world sunscreen usage
Our recommendations need to be based on real-world usage, not theory.
One of the first studies to demonstrate the real-world benefits of using very high SPF sunscreens was a split-face study in 2010 of 58 skiers comparing SPF50 and SPF85 sunscreens. This study had a number of limitations, nonetheless, it found 8 cases of sunburn on the SPF50 side compared to 1 case in the SPF85 group.
In 2020, a randomised, double-blind clinical trial compared the efficacy of SPF100+ to SPF50+ sunscreen in real-world use using a split body study design. It found after a five-day beach holiday, 56% of people had sunburn on the SPF50+ side of their body compared to 7% on the SPF100+ side. Sunburn also occurred earlier (day 1) on the SPF50+ side compared to the SPF100+ side (day 3).

Unfortunately, there were significant limitations to this study. It used different brands of sunscreen for SPF50+ (Banana Boat Sport Performance) and SPF100+ (Neutrogena Ultra Sheer Dry-Touch). They also used the labelled SPF ratings rather than testing the actual SPF of these products. Given the numerous recent cases of alleged SPF lab testing fraud and the subsequent variability in actual SPF as investigated by Consumer NZ, we find this to be a significant shortcoming. Although the products did share mostly similar ingredients – with higher concentrations in the SPF100+.
Consumer NZ’s most recent testing on Banana Boat SPF50+ (Daily Protect – different to the above study) suggested an actual SPF of 34. Consumer NZ’s testing also found that Neutrogena Ultra Sheer Dry-Touch Sunscreen SPF50+ met their labelled claim.
A further limitation of the 2020 study, was there was no comment regarding the different formulations of the products as this could have also introduced several biases. For example:
- Was one product easier to spread or less sticky resulting in more cream being applied and more evenly?
- Was one product more waterproof?
Nonetheless, several other subsequent studies have also shown very high SPF sunscreens to be beneficial. Even though these studies have been a little flawed, there is growing evidence that very high SPF sunscreens provide better protection, in real-world use.
Of course, the expectation is that the very high SPF creams can provide some compensation for people not applying it thick enough.
Split face sunscreen studies
Split-face (split-body) studies are designed to reduce variability within an individual.
In sunscreen studies, the aim is to eliminate the variability of sunscreen use between different individuals. The assumption is that a particular individual would apply the same amount of sunscreen to both sides of the face.
Of course, the goal is to measure the difference between SPF50 and SPF100 sunscreen in real-world usage.
Other factors affecting real-life SPF
There are several other factors that influence the real-life SPF:
Application of sunscreen
- Rubbing sunscreen during application reduces actual SPF by 20% when compared to gently applying.
- Sunscreens with better formulations that are easier to apply have less variability in the thickness of their application and real-world protection. Very high SPF (thicker & stickier) sunscreens may be more difficult to apply.
- Pump dispensers induce people to apply more cream compared to squeeze bottles and roll-ons.
- Dressing within 8 minutes of application will reduce the effect of the SPF when the cream is applied thicker than 1 mg/cm2. However, it has no effect if it’s applied less than 1 mg/cm2, presumably because there is little sunscreen to rub off.
- Studies have shown that intense education and demonstration regarding the appropriate quantity to apply does improve application amounts. However, at most, it still only reached 0.9-1.13 mg/cm2.
- Double application of sunscreen within 20 minutes is recommended. However, this is an attempt to get the application amount closer to 2 mg/cm2. There is no difference in protection from 2 applications of 1 mg/cm2 when compared to one application of 2 mg/cm2.
Water resistance of sunscreen
- Water and sand reduce its efficacy by about 30%.
- The application of sunscreen to skin that has previously had a cosmeceutical applied (eg. moisturiser) also significantly reduces water resistance.
Broad spectrum sunscreen
In Australia/New Zealand there is no numerical grading system for UVA. Sunscreens that are labelled as broad-spectrum must have UVA protection that must be at least one-third of the UVB SPF label.

Safety
Inorganic ingredients
Most inorganic sunscreens have a good safety record and do not exhibit significant absorption. With the increasing public concern about nanoparticles, several studies have assessed the absorption of inorganic nanoparticle ingredients and found no significant absorption:
- Zinc oxide does not appear to penetrate the epidermis (the most superficial layer of the skin). This was not affected by exposure to water.
- Titanium dioxide can penetrate the dermis (one layer deeper than the epidermis) but around hair follicles only. The amounts were tiny – approximately 0.00014% of the applied sunscreen and this is considered insignificant and of no consequence.
Organic ingredients
Organic ingredients do appear to result in systemic absorption, including into blood. A study to demonstrate the effect of maximal usage scenarios (four applications to 75% of the skin per day for four days) showed systemic absorption in amounts greater than 0.5 ng/mL. The sunscreen was applied 2 mg/cm2 per the testing recommendations. Furthermore, these ingredients had long elimination half-lives (mostly 24-42 hours, some up to 84 hours), meaning they accumulated with regular use.
Clearly, people use far less than these quantities, however, it demonstrates the need for further testing to determine the significance of this systemic absorption. We want to be clear that there is no evidence that these ingredients are harmful to systemic absorption. Nonetheless, if people are concerned they should consider using sunscreens with inorganic ingredients.
Environmental effects
There have been concerns that sunscreens potentially have a detrimental effect on marine ecosystems. Laboratory simulations have demonstrated that some UV filters, particularly oxybenzone could be toxic to anemones and coral resulting in their death and coral bleaching when exposed to UV light. However, it is uncertain how significant this is in actual coral reefs as the amount of UV that reaches these species underwater is variable.

Nonetheless, the National Oceanic and Atmospheric Administration (NOAA) lists the following ingredients as potentially harmful to marine life:
- 3-benzlidene camphor
- 4-methylbenzlidene camphor (enzacamene)
- octocrylene
- benzophenone-1
- benzophenone-2
- OD-PABA
- nano-titanium dioxide
- nano-zinc oxide
- octinoxate
- oxybenzone
Sunscreen for children
Children’s skin is thinner and more permeable than adult skin, so some have raised the concern of systemic absorption of sunscreens in children. They also have a higher risk of developing reactions, particularly to organic ingredients. However, this needs to be balanced against the higher susceptibility of their skin to sunlight as well as the fact that UV damage during childhood has a substantially higher impact on skin cancer development compared to adult UV damage.
There is also no evidence to say sunscreens shouldn’t be used on children and no evidence of toxicity with its ingredients.
Allergies
Most ingredients that cause sunscreen allergies are no longer used. Oxybenzone is the most commonly used UVA filter and the most common cause of allergic reactions (estimated rate is < 0.1%).
What about vitamin D?
There is a perception that using sunscreen will cause a vitamin D deficiency. While this perception is likely incorrect, the explanation is complicated. To start with, sunscreen use is unlikely to cause a vitamin D deficiency, however, it does reduce vitamin D synthesis by up to 50%.

Randomised controlled trials have demonstrated that daily sunscreen use does not affect vitamin D levels. However, this often-quoted study was performed during summer in Australia (high UV index) where vitamin D synthesis was likely to have been downregulated by the body as the stores would have been full.
Vitamin D synthesis is dependent on ultraviolet B and not UVA. UVB levels correlate linearly with the UV index, whereas UVA levels are impacted by a number of variables. Furthermore, there seems to be saturation of vitamin D synthesis, meaning a large UV exposure will only produce so much vitamin D. Whereas smaller, regular UV exposures produce more vitamin D for the same overall UV dose. Once vitamin D levels reach a certain point, further synthesis is down-regulated and production slows.
Concerningly, studies have shown that vitamin D synthesis in skin without sunscreen correlates with DNA damage which is a precursor to skin cancer and photoaging. Other studies have demonstrated that sunscreen use reduces vitamin D synthesis by up to 50% while at the same time substantially reducing DNA damage.
There is minimal UVB below a UV index of 3, meaning that there will be little, if any vitamin D synthesis at these levels which includes the winter months. This means that in winter, sunscreen use provides beneficial protection against DNA damage without impacting vitamin D synthesis at these levels.
In Auckland, the average peak UV index is only significantly below 3 for June and July. Whereas for Christchurch it is from May through August.
So what does all this mean?
- In summer, sunscreen use is very unlikely to impact vitamin D levels as synthesis tends to saturate stores. At the same time, it will substantially reduce DNA damage and reduce the risk of skin cancer.
- At UV index levels of 3 and below there is minimal if any vitamin D synthesis – sunscreen use can’t have a significant impact on negligible synthesis. However, it will still protect against DNA damage when exposed for 60 minutes or more.
- At other times, remember:
- Vitamin D stores last for about two months (Auckland’s UV peak UV index is only below 3 for about two months of the year).
- Sunscreen reduces synthesis by about 50% but reduces DNA damage by a much larger amount.
What are the key takeaways?
- It is important to not lose sight of the fact that sunlight is a carcinogen and it does very real damage that leads to skin cancer – which can be life-threatening. There is no safe level of sunlight exposure thus sun protection should be a priority. Some compare the sun to a giant nuclear fusion reactor emitting its radiation glow worldwide to help motivate people to practice better sun protection.
- New Zealand has very high rates of skin cancer that continues to kill over 500 people every year.
- We recommend daily sun protection throughout the year and if required, take a vitamin D supplement like many dermatologists worldwide.
References
- Van der Pols, J. C., Williams, G. M., Pandeya, N., Logan, V., & Green, A. C. (2006). Prolonged Prevention of Squamous Cell Carcinoma of the Skin by Regular Sunscreen Use. Cancer Epidemiology Biomarkers & Prevention, 15(12), 2546-2548. doi: 10.1158/1055-9965.epi-06-0352
- Green, A. C., Williams, G. M., Logan, V., & Strutton, G. M. (2011). Reduced Melanoma After Regular Sunscreen Use: Randomized Trial Follow-Up. Journal of Clinical Oncology, 29(3), 257-263. doi: 10.1200/jco.2010.28.7078
- Marks, R. (1995). The Effect of Regular Sunscreen Use on Vitamin D Levels in an Australian Population. Archives of Dermatology, 131(4), 415. doi: 10.1001/archderm.1995.01690160043006
- Young, A. R., Sheehan, J. M., Chadwick, C. A., & Potten, C. S. (2000). Protection by Ultraviolet A and B Sunscreens Against In Situ Dipyrimidine Photolesions in Human Epidermis is Comparable to Protection Against Sunburn. Journal of Investigative Dermatology, 115(1), 37-41. doi: 10.1046/j.1523-1747.2000.00012.x
- Neale, R., Williams, G., & Green, A. (2002). Application Patterns Among Participants Randomized to Daily Sunscreen Use in a Skin Cancer Prevention Trial. Archives of Dermatology, 138(10). doi: 10.1001/archderm.138.10.1319
- Petersen, B., & Wulf, H. C. (2014). Application of sunscreen – theory and reality. Photodermatology, Photoimmunology & Photomedicine, 30(2-3), 96-101. doi: 10.1111/phpp.12099
- Consumer NZ. Sunscreen test results. June 2022; Consumer NZ: Sunscreen Test Results
- Kohli, I., Nicholson, C. L., Williams, J. D., Lyons, A. B., Seo, I., Maitra, P., et al. (2019). Greater efficacy of SPF 100+ sunscreen compared to SPF 50+ in sunburn prevention during five consecutive days of sunlight exposure: A Randomized, Double-Blind Clinical Trial. Journal of the American Academy of Dermatology. doi: 10.1016/j.jaad.2019.09.018
- Sander, M., Sander, M., Burbidge, T., & Beecker, J. (2020). The efficacy and safety of sunscreen use for the prevention of skin cancer. Canadian Medical Association Journal, 192(50), E1802-E1808. doi: 10.1503/cmaj.201085
- Matta, M. K., Zusterzeel, R., Pilli, N. R., Patel, V., Volpe, D. A., Florian, J., & Strauss, D. G. (2019). Effect of Sunscreen Application Under Maximal Use Conditions on Plasma Concentration of Sunscreen Active Ingredients. JAMA. doi: 10.1001/jama.2019.5586
- Agin, P. P., Ruble, K., Hermansky, S. J., & McCarthy, T. J. (2008). Rates of allergic sensitization and irritation to oxybenzone-containing sunscreen products: a quantitative meta-analysis of 64 exaggerated use studies. Photodermatology, Photoimmunology & Photomedicine, 24(4), 211-217. doi: 10.1111/j.1600-0781.2008.00363.x
- Yap, F. H., Chua, H. C., & Tait, C. P. (2017). Active sunscreen ingredients in Australia. Australasian Journal of Dermatology, 58(4), e160-e170. doi: 10.1111/ajd.12597
- Federal Drug Administration. Sunscreen Drug Products for Over-the-Counter Human Use; Proposed Amendment of Final Monograph. 27 August, 2007; National Archives Federal Register

