Photodynamic therapy (PDT) is a treatment that combines the use of a photo (light)-sensitising cream with a light source such as a laser. This causes a reaction that selectively kills cancerous cells in skin cancer.
How Does Photodynamic Therapy Work?
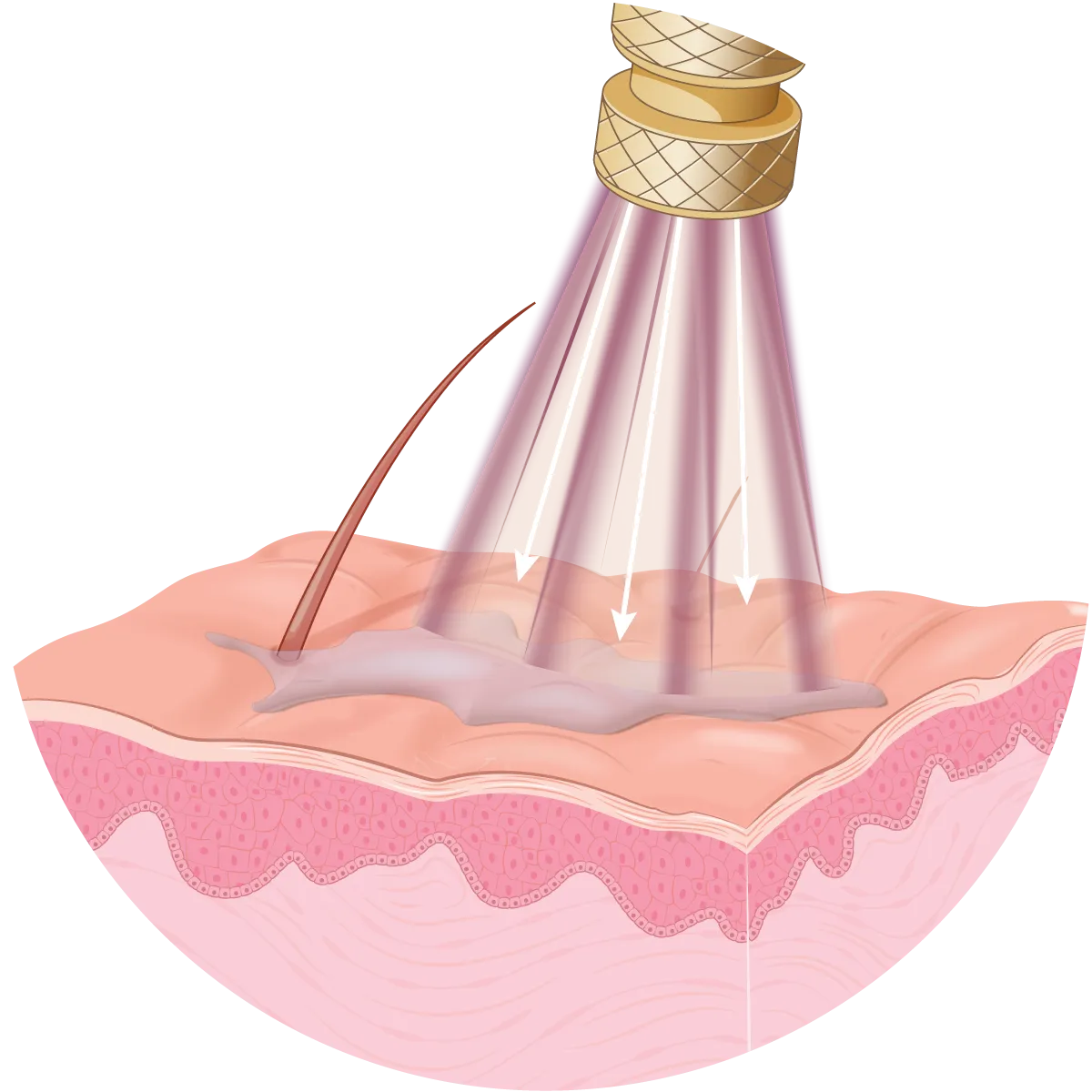
PDT involves applying a photosensitising agent to the treatment area. This gets absorbed into the skin during the incubation period, typically a few hours. The area is then irradiated at a wavelength that matches the photosensitiser, traditionally by a laser light.
Preparation
The skin may be prepared prior to photodynamic therapy to improve the absorption of the sensitising agent. The skin is designed to keep things out of the body, so the biggest challenge for PDT is achieving adequate penetration of photosensitiser into the skin.
The skin may be prepared prior to treatment to improve penetration into the skin and tumour. There are several options to achieve this:
- Keratolytic creams like salicylic acid for several days prior to treatment. This can help descale and exfoliate the skin.
- Scraping / curettage of the treatment area on the day of treatment.
- More recently preparation with fractional ablative lasers to create micro-channels into the skin. This is referred to as laser-assisted photodynamic therapy.
Photosensitisation
A photosensitising cream is then applied to the treatment area. This is allowed to absorb into the skin for an incubation period. This is typically around 3-6 hours. This prolonged incubation period allows the photosensitising agent to concentrate within the tumour cells. Photosensitisers preferentially localise in to cancerous cells allowing for targeted treatment.
There are several different types of photosensitisers that are commonly used during PDT:
- Methyl aminolevulinic acid, commonly known as Metvix
- Aminolevulinic acid, commonly known as ALA
Activating the Photosensitiser
The photosensitising agent is then activated by a light source that matches the absorption wavelength of the photosensitiser. This causes the photosensitiser to preferentially absorb the energy from the light source, resulting in selective damage to the treatment area and abnormal cells.
Activating light sources:
- Red laser is used for Metvix, usually for several minutes.
- Blue laser for ALA for several minutes.
- Sunlight can also be used, but typically takes a few hours of exposure. Results can also be variable based on cloud cover and UV intensity on the treatment day. Sunlight PDT is more practical when treating a large area such as a field treatment e.g. the whole face.
What Can Photodynamic Therapy Treat?
Photodynamic therapy (PDT) is mostly used to treat superficial basal cell carcinomas (sBCCs) and actinic field damage. However, published studies (and our own experience) have demonstrated that it is less effective than alternative (and often cheaper) treatment options such as Efudix.
PDT has recently been shown to be effective for other indications:
- Skin rejuvenation
- Moderate acne
- Psoriasis
- Folliculitis
- Fungal infections
How Effective is Photodynamic Therapy?
PDT is effective for a range of skin lesions. However, the limitations of treatment mean that it can only help with superficial lesions.1Braathen LR, Szeimies RM, Basset-Seguin N, et al. Guidelines on the use of photodynamic therapy for nonmelanoma skin cancer: an international consensus. International Society for Photodynamic Therapy in Dermatology, 2005. J Am Acad Dermatol. 2007;56(1):125-143. doi:10.1016/j.jaad.2006.06.006,2Nestor MS, Gold MH, Kauvar AN, et al. The use of photodynamic therapy in dermatology: results of a consensus conference. J Drugs Dermatol. 2006;5(2):140-154.
- Actinic keratoses can be treated with PDT. Several earlier studies have demonstrated response rates of around 70-100%.3Freeman M, Vinciullo C, Francis D, et al. A comparison of photodynamic therapy using topical methyl aminolevulinate (Metvix) with single cycle cryotherapy in patients with actinic keratosis: a prospective, randomized study. J Dermatolog Treat. 2003;14(2):99-106. doi:10.1080/09546630310012118,4Pariser DM, Lowe NJ, Stewart DM, et al. Photodynamic therapy with topical methyl aminolevulinate for actinic keratosis: results of a prospective randomized multicenter trial. J Am Acad Dermatol. 2003;48(2):227-232. doi:10.1067/mjd.2003.49,5Morton C, Horn M, Leman J, et al. Comparison of topical methyl aminolevulinate photodynamic therapy with cryotherapy or Fluorouracil for treatment of squamous cell carcinoma in situ: Results of a multicenter randomized trial. Arch Dermatol. 2006;142(6):729-735. doi:10.1001/archderm.142.6.729,6Szeimies RM, Karrer S, Radakovic-Fijan S, et al. Photodynamic therapy using topical methyl 5-aminolevulinate compared with cryotherapy for actinic keratosis: A prospective, randomized study. J Am Acad Dermatol. 2002;47(2):258-262. ,7Szeimies RM, Stockfleth E, Popp G, et al. Long-term follow-up of photodynamic therapy with a self-adhesive 5-aminolaevulinic acid patch: 12 months data. Br J Dermatol. 2010;162(2):410-414. doi:10.1111/j.1365-2133.2009.09377.x
- Actinic field damage: Disappointingly, a study published in 2019 demonstrated that only 38% of people maintained adequate clearance twelve months after treatment.8Jansen MHE, Kessels JPHM, Nelemans PJ, et al. Randomized Trial of Four Treatment Approaches for Actinic Keratosis. N Engl J Med. 2019;380(10):935-946. doi:10.1056/NEJMoa1811850
- Squamous cell carcinoma in situ has also been effectively treated with PDT. Response rates of about 50-90% have been reported.9Salim A, Leman JA, McColl JH, Chapman R, Morton CA. Randomized comparison of photodynamic therapy with topical 5-fluorouracil in Bowen’s disease. Br J Dermatol. 2003;148(3):539-543. doi:10.1046/j.1365-2133.2003.05033.x,10Morton CA. Methyl aminolevulinate: actinic keratoses and Bowen’s disease. Dermatol Clin. 2007;25(1):81-87. doi:10.1016/j.det.2006.09.009,11Morton CA, Whitehurst C, Moseley H, McColl JH, Moore JV, Mackie RM. Comparison of photodynamic therapy with cryotherapy in the treatment of Bowen’s disease. Br J Dermatol. 1996;135(5):766-771.,12Szeimies RM, Morton CA, Sidoroff A, Braathen LR. Photodynamic therapy for non-melanoma skin cancer. Acta Derm Venereol. 2005;85(6):483-490. doi:10.1080/00015550510044136
- Superficial basal cell carcinomas (BCCs) have also been treated with PDT. About 70-90% of these lesions respond to treatment, however, about 10% return (recur) within four years.13Zeitouni NC, Shieh S, Oseroff AR. Laser and photodynamic therapy in the management of cutaneous malignancies. Clin Dermatol. 2001;19(3):328-338. doi:10.1016/s0738-081x(01)00170-5
Laser-Assisted Photodynamic Therapy
Laser-assisted photodynamic therapy involves preparing the skin by creating numerous micro-channels deeper into the skin prior to treatment with PDT. This is normally achieved with ablative fractional lasers. The goal is achieve deeper penetration of the photosensitiser into the skin, boosting the efficacy of treatment.
Some small studies have demonstrated that laser-assisted PDT may boost treatment efficacy by 15-50% when compared to traditional PDT.14Lonsdorf AS, Keller A, Hartmann J, Enk AH, Gholam P. Ablative Fractional Laser-assisted Low-irradiance Photodynamic Therapy for Treatment of Actinic Keratoses in Organ Transplant Recipients: A Prospective, Randomized, Intraindividual Controlled Trial. Acta Derm Venereol. 2022;102:adv00694. Published 2022 Apr 13. doi:10.2340/actadv.v102.1057,15Wang JV, Griffin TD. Fractional Ablative Laser-Assisted Photodynamic Therapy as Field Treatment for Actinic Keratoses: Our Anecdotal Experience. Skinmed. 2020;18(4):214-216. Published 2020 Aug 1.,16Gu X, Zhao S, Shen M, Su J, Chen X. Laser-assisted photodynamic therapy vs. conventional photodynamic therapy in non-melanoma skin cancers: Systematic review and meta-analysis of randomized controlled trials. Photodermatol Photoimmunol Photomed. 2021;37(6):556-558. doi:10.1111/phpp.12700
Summary
While photodynamic therapy is effective, there is significant time investment and cost involved in administering treatment. Efficacy is similar to much cheaper treatment options such as Efudix treatment. In some studies it has been shown to be less effective than Efudix.
Overall, it is ethically difficult to justify the use of photodynamic therapy, given the cost and time involved. This is particularly the case when compared to the low cost and similar efficacy of other treatments like Efudix field treatment. Especially when Efudix can be done repeatedly to boost efficacy for a similar cost.
We generally don’t recommend PDT at Skintel as there are much more effective & cheaper options.
However, there may be a role for the more effective laser-assisted PDT for those that don’t respond adequately to Efudix field treatment.
References
- 1Braathen LR, Szeimies RM, Basset-Seguin N, et al. Guidelines on the use of photodynamic therapy for nonmelanoma skin cancer: an international consensus. International Society for Photodynamic Therapy in Dermatology, 2005. J Am Acad Dermatol. 2007;56(1):125-143. doi:10.1016/j.jaad.2006.06.006
- 2Nestor MS, Gold MH, Kauvar AN, et al. The use of photodynamic therapy in dermatology: results of a consensus conference. J Drugs Dermatol. 2006;5(2):140-154.
- 3Freeman M, Vinciullo C, Francis D, et al. A comparison of photodynamic therapy using topical methyl aminolevulinate (Metvix) with single cycle cryotherapy in patients with actinic keratosis: a prospective, randomized study. J Dermatolog Treat. 2003;14(2):99-106. doi:10.1080/09546630310012118
- 4Pariser DM, Lowe NJ, Stewart DM, et al. Photodynamic therapy with topical methyl aminolevulinate for actinic keratosis: results of a prospective randomized multicenter trial. J Am Acad Dermatol. 2003;48(2):227-232. doi:10.1067/mjd.2003.49
- 5Morton C, Horn M, Leman J, et al. Comparison of topical methyl aminolevulinate photodynamic therapy with cryotherapy or Fluorouracil for treatment of squamous cell carcinoma in situ: Results of a multicenter randomized trial. Arch Dermatol. 2006;142(6):729-735. doi:10.1001/archderm.142.6.729
- 6Szeimies RM, Karrer S, Radakovic-Fijan S, et al. Photodynamic therapy using topical methyl 5-aminolevulinate compared with cryotherapy for actinic keratosis: A prospective, randomized study. J Am Acad Dermatol. 2002;47(2):258-262.
- 7Szeimies RM, Stockfleth E, Popp G, et al. Long-term follow-up of photodynamic therapy with a self-adhesive 5-aminolaevulinic acid patch: 12 months data. Br J Dermatol. 2010;162(2):410-414. doi:10.1111/j.1365-2133.2009.09377.x
- 8Jansen MHE, Kessels JPHM, Nelemans PJ, et al. Randomized Trial of Four Treatment Approaches for Actinic Keratosis. N Engl J Med. 2019;380(10):935-946. doi:10.1056/NEJMoa1811850
- 9Salim A, Leman JA, McColl JH, Chapman R, Morton CA. Randomized comparison of photodynamic therapy with topical 5-fluorouracil in Bowen’s disease. Br J Dermatol. 2003;148(3):539-543. doi:10.1046/j.1365-2133.2003.05033.x
- 10Morton CA. Methyl aminolevulinate: actinic keratoses and Bowen’s disease. Dermatol Clin. 2007;25(1):81-87. doi:10.1016/j.det.2006.09.009
- 11Morton CA, Whitehurst C, Moseley H, McColl JH, Moore JV, Mackie RM. Comparison of photodynamic therapy with cryotherapy in the treatment of Bowen’s disease. Br J Dermatol. 1996;135(5):766-771.
- 12Szeimies RM, Morton CA, Sidoroff A, Braathen LR. Photodynamic therapy for non-melanoma skin cancer. Acta Derm Venereol. 2005;85(6):483-490. doi:10.1080/00015550510044136
- 13Zeitouni NC, Shieh S, Oseroff AR. Laser and photodynamic therapy in the management of cutaneous malignancies. Clin Dermatol. 2001;19(3):328-338. doi:10.1016/s0738-081x(01)00170-5
- 14Lonsdorf AS, Keller A, Hartmann J, Enk AH, Gholam P. Ablative Fractional Laser-assisted Low-irradiance Photodynamic Therapy for Treatment of Actinic Keratoses in Organ Transplant Recipients: A Prospective, Randomized, Intraindividual Controlled Trial. Acta Derm Venereol. 2022;102:adv00694. Published 2022 Apr 13. doi:10.2340/actadv.v102.1057
- 15Wang JV, Griffin TD. Fractional Ablative Laser-Assisted Photodynamic Therapy as Field Treatment for Actinic Keratoses: Our Anecdotal Experience. Skinmed. 2020;18(4):214-216. Published 2020 Aug 1.
- 16Gu X, Zhao S, Shen M, Su J, Chen X. Laser-assisted photodynamic therapy vs. conventional photodynamic therapy in non-melanoma skin cancers: Systematic review and meta-analysis of randomized controlled trials. Photodermatol Photoimmunol Photomed. 2021;37(6):556-558. doi:10.1111/phpp.12700